Humana Gold Prior Authorization List: Navigating the Maze
So, you're a Humana Gold member, and you've heard whispers of this mythical beast: the prior authorization list. Don't worry, you're not alone. This list, this gatekeeper of medical procedures and medications, can seem daunting. But is it really that bad? Let's dive into the world of Humana Gold prior authorization and uncover what it's all about.
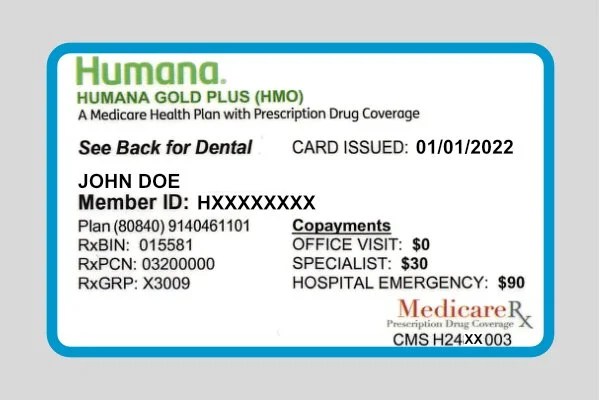
Essentially, a Humana Gold prior authorization, sometimes called pre-authorization, is like getting permission from Humana before receiving certain medical services or prescriptions. Think of it as a checkpoint to ensure the treatment is medically necessary and covered under your plan. Sounds simple enough, right? Well, the devil is often in the details. Finding the actual list of services and drugs requiring pre-authorization can feel like searching for a needle in a haystack.
Navigating the Humana Gold prior authorization process can be tricky. Where do you even start? The Humana website is a good starting point, but let's be honest, it can be a labyrinth of information. You might spend hours clicking through pages, only to end up more confused than before. Talking to a Humana representative is another option, but sometimes you get different answers depending on who you talk to. It's all a bit, shall we say, frustrating.
The history of prior authorizations is rooted in cost containment. Insurance companies introduced them as a way to manage healthcare expenses by ensuring that only medically necessary treatments are approved. Makes sense in theory, but in practice, it can create roadblocks for patients who need timely care. This is particularly true for those with chronic conditions who require ongoing treatments and medications.
The importance of understanding Humana's prior authorization requirements can't be overstated. Without pre-authorization, you could be stuck with a hefty bill. Imagine needing a specific medication, only to find out after the fact that it wasn't pre-authorized. Talk about a surprise no one wants! That’s why taking the time to understand the ins and outs of this process is crucial.
One benefit of prior authorizations is that it can help prevent unnecessary procedures and prescriptions, potentially saving you money in the long run. For example, if a less expensive, equally effective treatment is available, Humana might steer you toward that option. Another benefit is that it can help ensure you're receiving the right care for your condition. By reviewing the medical necessity of a treatment, Humana can help prevent potential complications or adverse reactions. Finally, while the process can be cumbersome, it provides a clear pathway for accessing covered services.
To navigate this system effectively, start by contacting Humana directly or visiting their website. Look for the "prior authorization" or "pre-authorization" section. You can also ask your doctor's office for assistance. They often handle prior authorization requests on behalf of their patients. Keep a record of your communications with Humana, including reference numbers and dates.
Advantages and Disadvantages of Humana Gold Prior Authorizations
| Advantages | Disadvantages |
|---|---|
| Cost containment | Delayed treatment |
| Ensures medically necessary treatment | Administrative burden |
| Can help prevent adverse reactions | Potential denial of necessary care |
A key best practice is to start the prior authorization process early. Don't wait until the last minute. Give yourself plenty of time, especially for complex procedures or medications. Another tip is to work closely with your doctor's office. They can be your best allies in navigating the prior authorization maze. Keep detailed records of everything, and don't be afraid to ask questions.
Frequently asked questions about Humana Gold prior authorizations include: How do I find the list of services requiring prior authorization? What if my prior authorization request is denied? How long does the process take? Who can I contact for help? What information do I need to provide? What happens after I submit a request? Can I appeal a denial? What are common reasons for denial?
One trick is to utilize online resources. Humana's website often has FAQs and helpful tools. Another is to connect with other Humana Gold members through online forums or support groups. They can share their experiences and offer valuable insights.
In conclusion, the Humana Gold prior authorization process can seem complex, but with the right knowledge and approach, it doesn't have to be a headache. By understanding the requirements, working closely with your doctor, and staying organized, you can navigate the system successfully and ensure you receive the care you need. Remember that prior authorizations are designed to manage costs and ensure appropriate treatment. While the process can be challenging, understanding its purpose and following best practices can greatly simplify the experience. Taking the time to learn the intricacies of Humana Gold prior authorization will ultimately empower you to advocate for your health and well-being. So, don't be intimidated. Be proactive, ask questions, and take control of your healthcare journey.
Unlocking opportunities crafting a winning sponsorship request letter
Marion county ks arrest records public access
Conquer march madness espn basketball bracket challenge